Stem Cell Injections for Osteoarthritis: A Patient's Guide
Living with the daily challenges of osteoarthritis often leads to a search for solutions that offer more than temporary symptom relief. For a growing number of individuals, stem cell injections for osteoarthritis represent a sophisticated, biologic therapy designed to work in harmony with your body’s innate healing capabilities. The objective is to enhance the internal joint environment, aiming to reduce discomfort and restore mobility.
A New Paradigm in Joint Health
Osteoarthritis (OA) is more than simple "wear and tear"; it is a progressive disease characterized by the gradual breakdown of the smooth, protective cartilage within a joint. This deterioration is the source of the familiar pain, stiffness, and loss of mobility that can significantly impact your quality of life.
For decades, conventional treatments have focused on managing these symptoms without addressing the underlying pathology within the joint. This is where the philosophy of regenerative medicine offers a paradigm shift. Instead of merely masking pain, the goal is to introduce powerful biologic components that can help cultivate a healthier, more balanced environment within the joint itself.
A New Approach To An Old Problem
The global prevalence of osteoarthritis is significant, affecting an estimated 250 million people worldwide. Given that cartilage has a very limited capacity for self-repair, standard treatments can often feel like temporary measures. Consequently, there is a strong demand for minimally invasive biologic options—such as stem cell injections—that may offer a path to reducing pain while helping to preserve joint structure. Explore further details on OA's global impact and treatment trends.
Our purpose with this guide is to provide you with a clear, sophisticated overview of how these advanced therapies function. We aim to equip you with a solid understanding of the science, the process, and the realistic potential of stem cell injections for osteoarthritis. We firmly believe that trusted, science-backed information is the key to making empowered decisions about your health.
We will navigate every key aspect of this treatment, from the fundamental science to the practical realities of the patient experience—including determining candidacy and understanding the recovery process.
By exploring this topic, you can build the confidence to engage in a well-informed dialogue with a specialist and determine if this path aligns with your personal joint health journey.
How Stem Cells Work to Address Joint Degeneration
To truly appreciate the mechanism of stem cell injections for osteoarthritis, it is necessary to move beyond the simplified notion that they merely "regrow" cartilage. The process is far more sophisticated. Their primary power lies in acting as intelligent biological directors within the joint, fundamentally shifting the environment from a state of chronic degradation toward one of active repair.
Consider them your body’s master repair crew. When introduced into a joint affected by osteoarthritis, their most immediate and powerful function is to orchestrate a healing response. They begin by calming the persistent, low-grade inflammation that drives both the pain and the cartilage destruction.
The Power of Cellular Communication
How do they achieve this? Through a remarkable process known as paracrine signaling. This is essentially a sophisticated form of cell-to-cell communication. The stem cells release a complex cocktail of beneficial molecules—including growth factors, cytokines, and exosomes—that instruct the surrounding cells on how to behave.
This cellular dialogue produces several critical effects within the joint:
- Powerful Anti-Inflammatory Action: The injected cells release proteins that directly counteract the inflammatory agents responsible for joint pain, swelling, and cartilage damage. This is often the first benefit patients experience.
- Modulating Immune Response: They help regulate the local immune response, preventing the body's own cells from perpetuating a destructive cycle.
- Protecting Existing Cartilage Cells: The growth factors secreted by stem cells act as a protective shield for your remaining cartilage cells (chondrocytes), supporting their survival and preserving existing joint structure.
The objective is not to create a brand-new joint surface overnight. Rather, it is to reset the joint's biology, fostering a healthier, less inflamed, and more functional space.
Different Cells for Different Jobs
The cells utilized in these treatments are almost exclusively Mesenchymal Stem Cells (MSCs). These are a specific type of adult stem cell renowned for their exceptional safety profile and regenerative potential. Sourced from tissues like bone marrow or umbilical cords, MSCs are ideally suited for orthopedic applications.
They are multipotent, meaning they have the capacity to differentiate into several types of specialized cells, including cartilage, bone, and fat cells. This versatility makes them highly effective within the joint environment. For those interested in the nuances of stem cell types, our guide on multipotent vs. pluripotent stem cells provides a more detailed exploration.
The modern understanding of stem cell therapy for joints is that the cells act more like conductors of an orchestra than builders on a construction site. They do not rebuild the entire structure from scratch; they guide the existing players to work in harmony, restoring balance and function.
It is this fundamental shift in the joint's internal environment that leads to the outcomes patients seek: reduced pain, improved mobility, and an enhanced quality of life. The treatment provides a powerful, targeted boost to your body’s own healing capacity.
From Theory to Tangible Results
The procedure itself is executed with precision. Using advanced imaging such as ultrasound, a physician delivers a concentrated dose of stem cells directly into the joint capsule. Once inside, the cells commence their work, initiating the cascade of anti-inflammatory and regenerative signals.
The result is a therapy that works on a biological level to address the root causes of osteoarthritis pain. It represents a move away from simply masking symptoms and toward actively improving the health and function of the joint itself.
Determining If You Are a Candidate for Stem Cell Therapy
While the science behind stem cell injections for osteoarthritis is compelling, it is not a universally applicable solution. A crucial first step involves a careful and thorough evaluation to determine if this specific therapy is the appropriate path for your joint health. This process is designed to match the right individual with the right treatment to achieve the best possible outcome.
The objective is to identify individuals whose specific condition aligns perfectly with the biological mechanisms of the therapy.
The Ideal Patient Profile
An ideal candidate is often an individual with mild-to-moderate osteoarthritis. These are typically people who retain a significant amount of cartilage in the joint, which provides a foundational structure for the stem cells to support and work with.
They have often explored first-line options—such as physical therapy, lifestyle modifications, or the temporary relief of cortisone injections—and are now seeking a more durable, minimally invasive option that could potentially delay or avoid major surgery.
The most successful outcomes are almost always seen in patients who are proactive about their health and possess realistic expectations. They understand that this is not a panacea, but a sophisticated therapy designed to improve the joint's biological environment, which in turn can lead to reduced pain and improved function over time.
A strong candidate typically meets the following criteria:
- Stage of Osteoarthritis: The condition is symptomatic but has not progressed to a severe, "bone-on-bone" state where cartilage is completely absent.
- Previous Treatments: Conservative options have been attempted but failed to provide sufficient or lasting relief.
- Health Status: The patient is in good overall health, free from active infections, certain blood disorders, or poorly controlled autoimmune conditions that could interfere with the treatment's efficacy.
- Commitment to Recovery: The individual is prepared and motivated to participate in a post-procedure rehabilitation program. Physical therapy is absolutely essential to maximize the benefits of the treatment.
Candidacy is determined less by chronological age and more by the biological and structural health of your joint. A comprehensive diagnostic workup is essential to obtain a complete picture before proceeding with any regenerative treatment.
This meticulous screening process ensures that stem cell injections for osteoarthritis are recommended for the patients who are most likely to benefit.
When Alternative Treatments Might Be Better
Conversely, stem cell therapy is not the optimal choice for everyone. In certain situations, other treatments, including traditional surgery, may offer a more predictable or effective result. It is vital to be transparent about these limitations.
Individuals who are generally not considered ideal candidates include those with:
- Advanced Osteoarthritis: In cases of end-stage, bone-on-bone arthritis, there is often insufficient cartilage remaining for the regenerative signals to have a meaningful impact. Joint replacement surgery may be a more definitive solution.
- Active Infections: Any infection, whether systemic or localized, must be fully resolved before considering a biologic injection, as introducing foreign material could lead to serious complications.
- Certain Medical Conditions: Specific autoimmune diseases or blood-related cancers may be contraindications. A detailed review of your medical history is a non-negotiable part of the screening process.
A comprehensive evaluation is the bedrock of responsible regenerative medicine. This always begins with a physical examination, a thorough review of your medical history, and, most importantly, advanced imaging like an MRI or specialized X-rays. These diagnostic tools allow your physician to assess the precise degree of cartilage loss, identify other structural issues like bone spurs or ligament tears, and ultimately confirm if the joint environment is truly suitable for stem cell therapy.
A summary of these factors can help clarify candidacy.
Candidacy Profile for Stem Cell Injections for Osteoarthritis
Ideal Candidate CharacteristicsPotential ContraindicationsMild to moderate osteoarthritis confirmed by imaging.Severe "bone-on-bone" osteoarthritis with complete cartilage loss.Joint pain and dysfunction impacting quality of life.Active systemic or local joint infection.Insufficient relief from conservative treatments (PT, NSAIDs).Certain blood cancers or disorders.Sufficient remaining cartilage to provide a scaffold for repair.Uncontrolled autoimmune diseases.Good overall health with no major underlying conditions.Known allergy to components of the injection.Realistic expectations and commitment to rehabilitation.Inability or unwillingness to participate in post-procedure PT.
Ultimately, a detailed consultation and diagnostic workup with an experienced physician is the only way to determine your suitability with certainty. This ensures that the treatment path you choose offers the highest probability of success for your unique situation.
The Patient Journey: From Consultation to Recovery
When you decide to explore stem cell injections for osteoarthritis, you deserve to feel confident and well-informed from the very first interaction. We have structured the entire process to be a clear, supportive partnership, beginning with an in-depth consultation and diagnostic workup. This is not merely a formality; it is a foundational step to confirm your candidacy and to customize a plan that aligns with your specific joint health needs.
Consider it a collaboration between you and our clinical team. Your comfort, safety, and understanding are paramount at every stage, guiding you from the initial assessment through a fully supported recovery.
The Initial Consultation and Diagnostic Phase
Your journey does not begin with an injection—it begins with a conversation. The initial consultation is a deep dive into your medical history, your symptoms, and the ways in which osteoarthritis affects your life. This is our opportunity to listen, to understand your goals, and to address your questions.
Following this discussion, we proceed to a precise diagnostic workup. This almost always includes advanced imaging, such as an MRI, to obtain a crystal-clear picture of your joint's internal condition. This allows us to see the exact degree of cartilage loss, identify any other issues contributing to your pain, and confirm that the joint environment is suitable for a successful regenerative outcome.
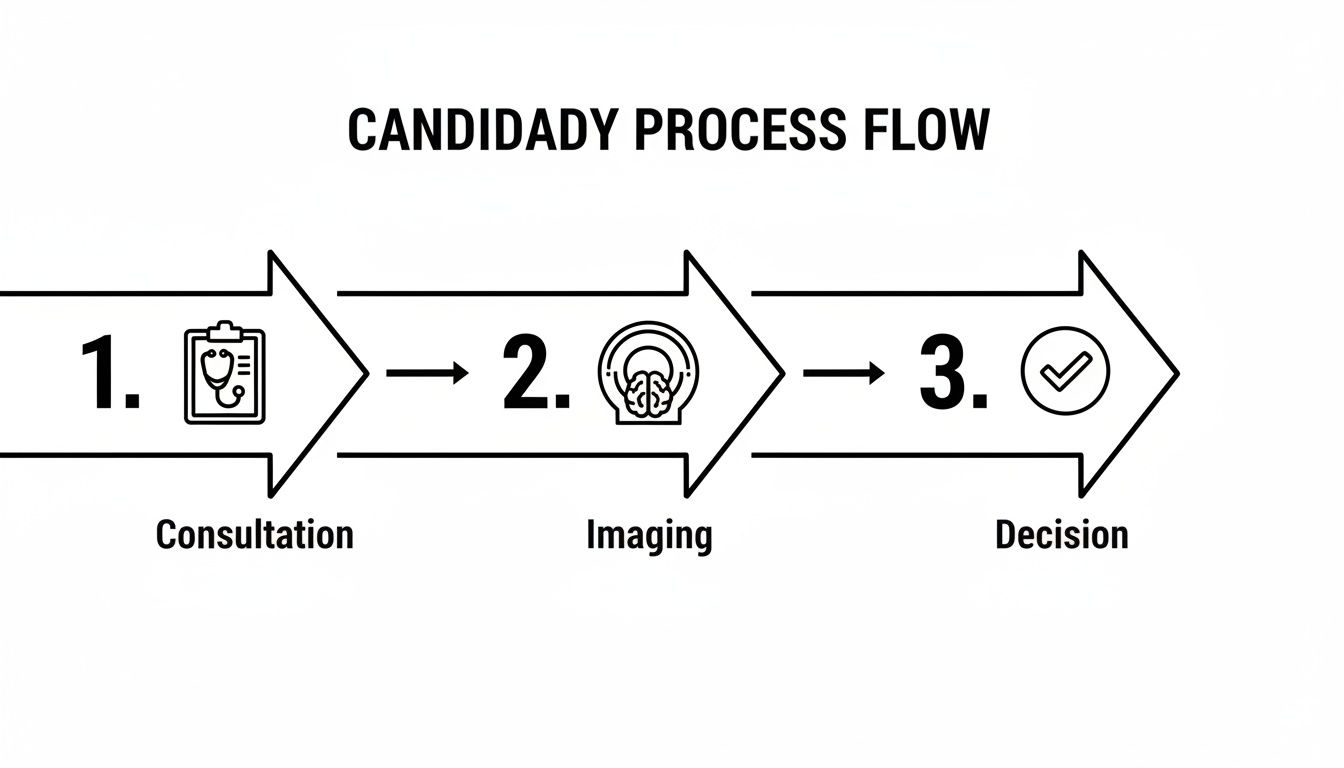
This graphic illustrates the structured steps we take to determine if this treatment is right for you.
This thorough evaluation is a critical quality control measure. It ensures that every patient who proceeds has been carefully vetted, which maximizes the potential for a positive result.
The Day of Your Procedure
On the day of the procedure, our focus is entirely on your comfort and safety. The process is minimally invasive and performed in a sterile clinical setting. Your physician will begin by administering a local anesthetic to numb the area, ensuring you experience little to no discomfort.
Precision is paramount. To achieve the best results, we deliver the stem cell injection using advanced ultrasound guidance. This technology provides your physician with a real-time view inside the joint, guaranteeing that the concentrated dose of stem cells is delivered exactly where it is needed most. The entire procedure is typically completed in under an hour.
The goal is to provide a powerful biological boost with minimal disruption to your body. Following a short observation period, you will be able to return home the same day.
The Crucial Recovery and Rehabilitation Period
The injection is only the first step. The subsequent recovery and rehabilitation phase is just as important as the procedure itself for achieving the best possible long-term outcome. We will provide you with a personalized recovery plan designed to protect the joint and create the ideal healing environment.
This plan is typically structured in a few key stages:
- Initial Rest Period: For the first few days, you will need to rest and limit activity. This allows the joint time to begin responding to the therapy.
- Gradual Re-engagement: Next, you will slowly reintroduce gentle movement and light, low-impact activities under our team's guidance.
- Structured Physical Therapy: This is a non-negotiable component of a successful recovery. A specialized physical therapy program is essential to restore strength, flexibility, and proper joint mechanics.
The synergy between the biological action of the stem cells and the mechanical support from rehabilitation is what drives optimal healing. One without the other is an incomplete approach.
This guided recovery provides the stem cells with the best possible opportunity to be effective. To learn more about how physical therapy and regenerative treatments work in concert, please see our guide on regenerative rehabilitation therapy.
The scale of knee osteoarthritis is immense, with approximately 1.9 million knee replacement surgeries performed in the U.S. in 2023 alone. This highlights the urgent need for less invasive options with lasting benefits. Promising research, such as a trial on an allogeneic stem cell product, reported a 58% sustained reduction in pain at 12 months post-injection, with some MRI scans suggesting an increase in cartilage volume. Long-term follow-up from similar studies indicates that the benefits from a single injection could persist for over four years, underscoring the durability that many patients seek.
Comparing Stem Cells, PRP, and Conventional Treatments
When navigating the complexities of joint pain, the array of treatment options can feel overwhelming. To make an informed decision for your health, it is essential to understand where stem cell injections for osteoarthritis fit within the broader therapeutic landscape. Each choice, from a simple cortisone injection to a full joint replacement, functions differently and carries its own set of expectations.
Let's examine them individually, so you can clearly see how regenerative medicine offers a fundamentally different approach.
Corticosteroid Injections: The Quick Fix
Corticosteroid injections are a common first-line intervention. These powerful anti-inflammatory drugs are delivered directly into the joint and act rapidly. The primary goal is to dramatically reduce the inflammation that drives pain and swelling in an arthritic joint. For many, a cortisone injection provides swift, welcome relief.
However, this effect is temporary, typically lasting only a few weeks or months. More importantly, corticosteroids do not address the underlying pathology or repair damaged cartilage. In fact, there is growing evidence that repeated injections may weaken cartilage over time, which is why their use is carefully managed. They are a short-term solution, not a long-term strategy.
Platelet-Rich Plasma (PRP): A Step Toward Healing
Platelet-Rich Plasma (PRP) is another biologic option that leverages your body's own healing capacity. A small sample of your blood is drawn, processed in a centrifuge to concentrate the platelets, and the resulting plasma is injected back into your joint. Platelets are rich in growth factors—powerful biochemical messengers that signal your body to initiate a repair process.
PRP is an excellent tool for reducing inflammation and fostering a healthier intra-articular environment. It is a definitive step up from cortisone because it aims to encourage healing rather than just mask symptoms. However, stem cell therapy advances this concept further. While PRP provides the "signals" for repair, stem cells function more like the "general contractors" of the project, capable of orchestrating a more complex, sustained, and powerful regenerative response.
Total Joint Replacement: The Definitive Surgical Option
For severe, "bone-on-bone" osteoarthritis, total joint replacement remains the gold standard. This major surgical procedure involves removing the worn-out joint surfaces and replacing them with a high-tech prosthesis made of metal and plastic. It is an undeniably effective method for eliminating pain and restoring function when a joint is too damaged for natural repair.
However, it is a significant undertaking. Joint replacement entails surgical risks, a long and often painful recovery, and a permanent alteration to your body. Stem cell therapy exists as a minimally invasive alternative for the right candidate—someone with mild-to-moderate arthritis who wishes to preserve their own joint and, ideally, delay or avoid the need for major surgery.
At its core, the distinction is simple. Conventional treatments focus on managing symptoms. Regenerative therapies like PRP and stem cell injections aim to change the joint environment to help the body heal itself.
It is also critical to maintain realistic expectations. While patient interest is high, the science continues to evolve. High-quality studies show that stem cell therapy for knee osteoarthritis is still considered investigational and has not consistently outperformed standard treatments. For instance, the multicenter MILES trial compared different cell injections to a simple corticosteroid shot. After one year, researchers found no significant difference in pain or function between the groups. Even on MRI, there were no major changes to the cartilage. This suggests the benefits may be more subtle than once hoped. You can learn more about the current market landscape and research findings here.
This table summarizes the key differences.
Treatment OptionPrimary MechanismBest ForKey ConsiderationCorticosteroid InjectionsPotent anti-inflammatoryRapid, short-term pain reliefEffects are temporary; repeated use is limited.PRP InjectionsUses growth factors to signal repairMild osteoarthritis, inflammationLess robust regenerative potential than stem cells.Stem Cell InjectionsOrchestrates a healing environmentMild-to-moderate osteoarthritisMinimally invasive; considered investigational.Total Joint ReplacementReplaces damaged joint with a prosthesisSevere, "bone-on-bone" osteoarthritisDefinitive solution; requires major surgery and recovery.
Ultimately, the optimal path forward depends on the advancement of your arthritis, your personal goals, and a candid discussion with a specialist who can help you weigh the true pros and cons of every option.
How to Choose a Reputable Stem Cell Clinic
When considering stem cell injections for osteoarthritis, the quality of your outcome is directly linked to the clinic you choose. In this rapidly advancing field, making a safe, informed decision is paramount. It is essential to vet potential providers with a critical eye to distinguish between legitimate medical institutions and those capitalizing on market trends.
Your search should begin with physician-led clinics, specifically those with board-certified specialists in disciplines such as orthopedics, sports medicine, or physical medicine. True experts in this domain will always perform injections using advanced imaging, like ultrasound, to guarantee the cells are delivered with pinpoint precision to the exact location within your joint.
This is not a luxury; it is a fundamental standard of care.
Verify Physician Credentials and Experience
When evaluating a clinic, begin with the practitioners. The physicians overseeing your care must possess extensive experience not only in their specialty but specifically in regenerative medicine. Do not hesitate to ask direct questions.
Here is what you should look for:
- Board Certification: This confirms the physician has met rigorous standards in a relevant specialty like orthopedics.
- Regenerative Medicine Training: Inquire about specific fellowships or advanced training they have completed in cellular therapies.
- Procedural Volume: How many procedures similar to yours has the doctor performed? Experience is a critical factor.
A transparent and confident physician will welcome these questions and be pleased to share their credentials. This level of openness is a strong indicator of a trustworthy practice.
Scrutinize Lab Quality and Cell Processing
The quality of the cells being injected is as critical as the skill of the physician administering them. A reputable clinic will be completely transparent about its cell sourcing and laboratory standards. The gold standard is a clinic with its own on-site, government-licensed laboratory.
The presence of an on-site, licensed, and ISO-certified lab ensures that the entire process—from cell sourcing and processing to final preparation—is handled under one roof, subject to strict, verifiable quality control measures. This minimizes risks and maximizes the quality of the biologic product.
This vertical integration is a major differentiator. It signifies that the clinic maintains full control over the safety, purity, and viability of the stem cells, which is absolutely essential for a safe and effective treatment. For those exploring international options, our guide to finding the best licensed stem cell clinic in Mexico offers more specific insights.
Finally, a clinic’s commitment to patient outcomes should be evident. The best centers actively track their patients' progress long-term. They should be prepared to discuss their results—both successes and limitations—in a realistic, data-driven manner. Conducting this due diligence empowers you to select a provider you can trust with your joint health, ensuring your care is not only advanced but also safe, precise, and genuinely focused on you.
Your Questions About Stem Cell Injections, Answered
Embarking on a new treatment is a significant decision, and it is natural to have questions. When the treatment is as advanced as stem cell injections for osteoarthritis, clear and straightforward answers are essential. Here, we address some of the most common questions from patients, providing the practical information you need to move forward with confidence.
We have curated concise responses to help you understand what to expect.
How Long Does It Take to See Results?
This is one of the most important questions patients ask. Because this therapy works by supporting your body’s own healing mechanisms, the results manifest gradually. It is best understood not as an overnight fix, but as a biological process of renewal.
Most of our patients begin to notice tangible improvements in pain and joint function within two to three months. These positive changes often continue to progress for six months or longer as the joint environment becomes healthier and more stable.
Is the Procedure Painful?
Patient comfort is a top priority. Prior to the injection, the area is thoroughly numbed with a local anesthetic, similar to what you might experience during a dental procedure.
This ensures the procedure itself involves minimal discomfort. Most individuals describe the sensation as a feeling of pressure rather than sharp pain. It is entirely normal to experience some soreness at the injection site afterward, but this typically subsides on its own within a few days.
The key takeaway is that the entire procedure is designed to be a minimally invasive experience. Our focus is on precision and comfort, helping you avoid the significant pain and lengthy recovery associated with major surgery.
Are Stem Cell Injections Covered By Insurance?
This is a practical and important consideration. Currently, most insurance providers in the United States and Canada classify stem cell therapy for osteoarthritis as an investigational treatment. For this reason, it is typically not a covered benefit.
This means the treatment is usually a self-pay procedure. Any reputable clinic will provide you with clear, transparent pricing information upfront. There should be no hidden costs or surprises, allowing you to make a fully informed financial decision.
At Longevity Medical Institute, we are committed to providing you with the highest standard of care in regenerative medicine. If you have further questions or are ready to explore if stem cell therapy is the right choice for you, we invite you to schedule a comprehensive consultation with our team of specialists.
Considering Stem Cell Therapy in Cabo San Lucas?
Cabo San Lucas is part of the greater Los Cabos medical corridor and serves patients traveling to the region for regenerative and longevity-focused care.
Longevity Medical Institute coordinates physician-supervised regenerative services for patients in Cabo San Lucas, emphasizing appropriate candidacy, clinical oversight, and informed decision-making. This approach allows patients to explore regenerative therapies within a regulated medical setting.
Learn more about regenerative medicine options near Cabo San Lucas.
Author
Dr. Kirk Sanford, DC — Founder & CEO, Longevity Medical Institute. Dr. Sanford focuses on patient education in regenerative and longevity medicine, translating complex therapies into clear, practical guidance for patients.
Medical Review
Dr. Félix Porras, MD — Medical Director, Longevity Medical Institute. Dr. Porras provides clinical oversight and medical review to help ensure accuracy, safety context, and alignment with current standards of care.
Last Reviewed: January 10, 2026
Short Disclaimer
This information is for educational purposes only and is not medical advice. It does not replace an evaluation by a qualified healthcare professional. For personalized guidance, please schedule a consultation.