Stem Cell Therapy for Rotator Cuff Tear: A Patient's Guide
When a rotator cuff tear results in persistent shoulder pain and weakness, the path forward can seem limited to managing symptoms or undergoing surgery. Stem cell therapy offers a sophisticated alternative—one that partners with your body to rebuild damaged tissue from within.
Unlike treatments that merely mask pain, this regenerative approach is designed to resolve the underlying injury by promoting natural tissue regeneration. It represents a powerful, minimally invasive option for patients seeking to avoid surgery and achieve lasting functional restoration.
Understanding Your Shoulder and the Rise of Regenerative Solutions
Your rotator cuff is a sophisticated system of four muscles and their tendons, working in harmony to stabilize your shoulder while enabling you to lift and rotate your arm. When these tendons tear—whether from an acute injury, chronic overuse, or gradual degeneration—the result is often persistent pain and frustrating functional limitations.
This is a remarkably common condition, affecting an estimated 20% of the population globally. For years, the standard of care has included physical therapy, corticosteroid injections, or arthroscopic surgery. While surgery can be effective, it is associated with a significant failure rate; studies reveal that anywhere from 30% to 94% of surgical repairs may re-tear, particularly in older patients or those with larger tears. You can explore a scholarly review of rotator cuff treatments to understand how the clinical science is evolving.
How Stem Cells Orchestrate Healing
This is where stem cell therapy for a rotator cuff tear charts a new course. Stem cells are best understood as your body’s own master conductors of tissue repair. When delivered with precision to the injured tendon, they do not simply fill a void. Instead, they orchestrate a powerful, localized healing response.
Here is their mechanism of action:
- Modulating Inflammation: Stem cells excel at resolving the chronic inflammation that often stalls the natural repair process.
- Recruiting Native Cells: They release signaling molecules that attract your body's own healing cells to the site of injury.
- Releasing Growth Factors: These potent proteins trigger the formation of new blood vessels and encourage existing cells to build strong, healthy tendon fibers.
The objective is not merely to patch the tear. It is to create the ideal biological environment for your shoulder to genuinely rebuild itself. This represents a fundamental shift from managing symptoms toward actively restoring tissue integrity.
By amplifying your body's innate healing capacity, this therapy is designed to restore shoulder function and deliver durable pain relief. To learn more about how this approach is applied across various conditions, you can review our guide on the fundamentals of stem cell therapy. It is a scientifically grounded path for patients who seek to heal effectively while avoiding more invasive procedures.
Comparing Rotator Cuff Treatment Approaches
When evaluating your options for a rotator cuff injury, it is beneficial to understand how stem cell therapy compares to conventional treatments. The table below outlines the key distinctions.
Treatment ApproachPrimary GoalInvasivenessTypical RecoveryStem Cell TherapyPromote tissue regeneration and healingMinimally invasive (injection)Gradual return to activity over weeksPhysical TherapyStrengthen surrounding muscles, improve mobilityNon-invasiveWeeks to months of consistent exerciseCorticosteroid InjectionsReduce inflammation and painMinimally invasive (injection)Temporary relief, often short-termSurgerySurgically reattach the torn tendonHighly invasive (arthroscopic or open)Months of recovery and rehabilitation
While each modality has its place, stem cell therapy is distinguished by its ability to directly address the biological cause of the injury. The focus extends beyond strength or pain relief—it is centered on true tissue repair.
How Stem Cells Actually Repair Damaged Tendons
To appreciate the promise of stem cell therapy for rotator cuff tears, one must look beyond the surface and understand the powerful biology at work. A common misconception is that these cells simply arrive at an injury site and transform into new tendon tissue. While differentiation is possible, their primary role is far more sophisticated—and ultimately, more impactful.
The cells utilized in our protocols, known as mesenchymal stem cells (MSCs), function as the body's elite project managers for tissue repair. Sourced from your own body—typically from bone marrow or adipose (fat) tissue—they are deployed to orchestrate a complex healing cascade. Rather than merely becoming new building blocks, they direct the entire reconstruction process.
This process is driven by the paracrine effect, a sophisticated form of cell-to-cell communication. The stem cells act as dispatchers, sending out highly specific instructions to all other cells involved in the healing process.
The Paracrine Effect Unpacked
Through the paracrine effect, stem cells release a potent cocktail of bioactive molecules—including growth factors, cytokines, and signaling proteins—into the local environment. These molecules serve as the "instructions" that guide the repair process.
This signaling cascade unfolds in several key steps:
- Resolving Inflammation: The first priority is to control inflammation. Chronic inflammation is a significant barrier to healing in a damaged rotator cuff. MSCs release powerful anti-inflammatory signals that calm irritated tissue, creating a stable environment where repair can begin.
- Recruiting Reinforcements: Next, stem cells act as beacons, sending chemical signals that attract your body's own native repair cells to the injury. This brings in the necessary workforce to clear away damaged debris and prepare the site for rebuilding.
- Initiating Reconstruction: Finally, they release growth factors that instruct local cells to produce new, healthy tendon tissue. These signals promote the formation of new blood vessels (angiogenesis) to deliver vital oxygen and nutrients, and they stimulate the production of collagen—the tough, fibrous protein that imparts strength to tendons.
In essence, stem cell therapy doesn’t just patch damaged tissue; it amplifies and intelligently directs your body's innate healing capacity. It's a powerful partnership between advanced medical science and your own biology.
Multipotent Cells: The Engine of Regeneration
The mesenchymal stem cells used in orthopedic treatments are multipotent. This means they possess the remarkable ability to develop into several different types of specialized cells, including cartilage, bone, and tendon cells. This versatility makes them powerful tools in regenerative medicine.
Their adaptability allows them to respond precisely to the needs of the damaged tissue. This is a key distinction in stem cell science. For a deeper understanding, you can explore our detailed comparison of multipotent versus pluripotent stem cells and their unique applications in medicine.
Ultimately, the goal of stem cell therapy for a rotator cuff tear is not just to patch an injury. By harnessing the paracrine effect and the multipotent nature of MSCs, the treatment aims to regenerate stronger, more resilient tendon tissue, restoring function and providing lasting relief from shoulder pain. It is a scientifically grounded approach focused on achieving true biological healing.
Translating Clinical Research into Patient Outcomes
While the science of stem cells is compelling, its true value lies in its clinical application for patients with real-world injuries. Clinical research serves as the critical bridge between a laboratory concept and a successful patient outcome. For rotator cuff tears, the data is increasingly clear: these therapies can lead to significant, measurable improvements.
The most robust studies focus not only on subjective reports of feeling better but also on tangible results like pain reduction, restored range of motion, and objective evidence of healing. Using advanced imaging such as MRI and ultrasound, clinicians can visualize a damaged, disorganized tendon gradually repairing itself, becoming stronger and more structurally sound.
This is not about collecting anecdotes. It is about building a solid, data-driven foundation to establish realistic patient expectations from a well-designed treatment protocol.
Evidence of Enhanced Healing and Durability
One of the most promising areas of research involves using stem cells to augment traditional surgery. The high re-tear rate following rotator cuff surgery has long been a challenge for orthopedic surgeons. Regenerative medicine is beginning to improve those odds.
A landmark study provided powerful long-term evidence. When surgeons augmented a standard arthroscopic repair with bone marrow stem cells, they observed a 100% healing rate. In the control group that received surgery alone, the rate was only 67%. Remarkably, this benefit was sustained at the 10-year follow-up.
Supporting this, real-world data from the Mayo Clinic showed that patients who received bone marrow concentrate during their rotator cuff repair were nearly three times less likely to require revision surgery. You can explore the detailed findings on BMSC augmentation here.
These studies converge on a single conclusion: stem cells create a more robust healing environment, leading to a more durable repair.
Key Measurable Outcomes in Clinical Trials
When researchers evaluate stem cell therapy for rotator cuff tears, they track specific, standardized metrics to ensure the results are objective and reliable.
- Pain Reduction: Using validated pain scales, studies consistently demonstrate that patients experience significant and lasting relief from shoulder pain.
- Functional Improvement: This is measured with shoulder-specific questionnaires that score a patient’s ability to perform daily activities, from combing their hair to lifting groceries. Results frequently show major gains in functional capacity.
- Tendon Integrity: Follow-up MRI scans provide visual confirmation of healing, showing a reduction in tear size and an improvement in tissue quality over time.
- Reduced Re-Tear Rates: As noted, adding stem cells to a surgical repair has been shown to dramatically lower the chances of the tendon failing again.
The combination of these outcomes—less pain, improved function, and visible tissue repair—makes a powerful case for using stem cells to achieve a more complete and lasting recovery from rotator cuff injuries.
Of course, success is contingent upon the specifics of the injury and the patient's overall health. However, the body of evidence continues to grow, reinforcing that expertly administered stem cell joint injections can be a cornerstone of modern orthopedic care. For a closer look, please review our guide on how stem cells are used in joint therapies. Our commitment to this evidence-based approach ensures our protocols are built not on theory, but on a solid foundation of proven clinical results.
Your Stem Cell Treatment Journey
Understanding the potential of stem cell therapy is the first step; knowing what the process entails provides the confidence to move forward. At Longevity Medical Institute, we have designed a clear, patient-centric journey focused on transparency, safety, and achieving the best possible outcome.
From your initial consultation to your final follow-up, our clinical team manages every stage. This is a partnership where we work with you to unlock your body's healing potential with precision and clinical expertise.
Comprehensive Evaluation and Candidacy
Your journey begins not with a procedure, but with a thorough conversation and a deep diagnostic evaluation. This is the foundation of a successful treatment, providing a complete, 360-degree view of your shoulder's condition. We go far beyond a standard physical exam, utilizing advanced imaging like MRI and high-resolution ultrasound to map the precise location and severity of your rotator cuff tear.
This detailed workup helps us confirm your candidacy for therapy. More importantly, it allows us to design a treatment plan tailored specifically to your anatomy and personal goals. This data-driven approach removes guesswork and sets the stage for a truly targeted treatment.
The Harvesting and Preparation Process
Once candidacy is confirmed, the next step is to collect your body’s own powerful regenerative cells. Depending on your personalized protocol, this will involve harvesting stem cells from either your adipose (fat) tissue or bone marrow. This minimally invasive procedure is performed in our clinic using local anesthesia to ensure your comfort.
Your sample is then immediately processed in our on-site, COFEPRIS-licensed laboratory. Here, our specialists use sophisticated techniques to isolate and concentrate the stem cells. This crucial step ensures the final preparation is a pure and potent dose, maximizing the regenerative potential of the cells.
Precision Injection and Post-Treatment Care
The final step is delivering the concentrated stem cells directly into the damaged rotator cuff tendon. To achieve absolute accuracy, our physicians use real-time ultrasound guidance. This technology acts as a GPS for the needle, allowing us to visualize the anatomical structures and place the cells precisely where your body needs them most. You can observe this meticulous process in our video on ultrasound-guided shoulder stem cell injections.
This commitment to precision is non-negotiable. Placing the cells in the exact location of the tear is critical for activating a localized healing response and achieving the best possible outcome.
Recent research continues to highlight the efficacy of this targeted, non-surgical approach. Adipose-derived stem cells (ADSCs), in particular, show incredible promise. One major review found that high-dose ADSC injections into partial-thickness rotator cuff tears led to significant improvements in shoulder function and strength for up to two years, with no serious adverse events reported.
Following your procedure, our team will provide a detailed post-treatment plan. This is your personal roadmap to recovery, designed to support the healing process and help you achieve lasting success.
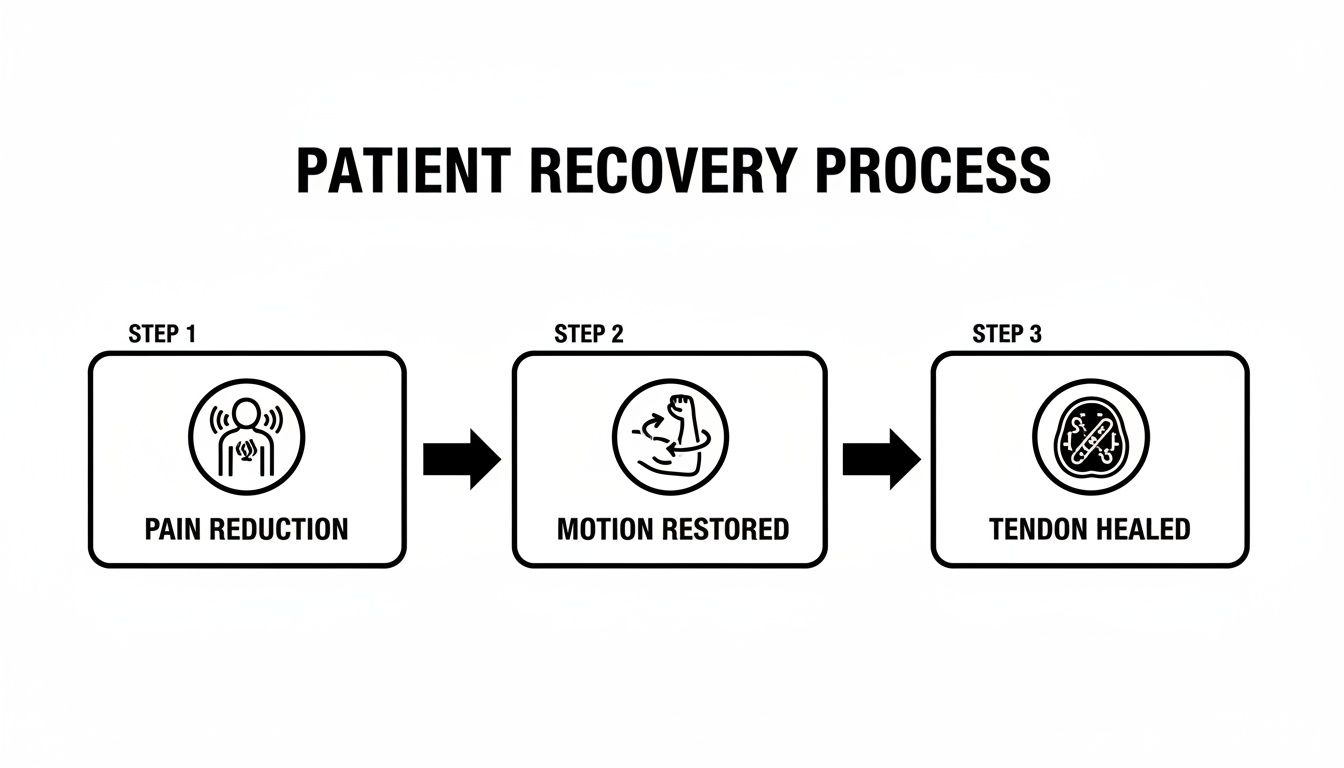
As illustrated, the recovery journey follows a clear progression: from initial pain relief to restored mobility and, ultimately, to the verified healing of the tendon itself.
Is Stem Cell Therapy Right for Your Rotator Cuff?
Not every shoulder injury is identical, and stem cell therapy is not a universal solution. The first and most critical step is always a meticulous and honest evaluation. Our objective is not to promote a procedure, but to determine if your specific injury and biology align with what regenerative medicine can offer. Establishing clear, realistic expectations is a cornerstone of our practice.
This process extends beyond identifying the source of your pain. It involves gaining a deep understanding of your shoulder’s structural health, reviewing your complete medical history, and discussing your personal recovery goals. By carefully matching the right patient to the right protocol, we can develop a targeted plan with the highest probability of success.
The Ideal Candidate Profile
While every individual is unique, clinical experience and a growing body of research have helped us define the profile of an ideal candidate. This therapy tends to be most effective for patients who fall into one or more of these categories.
- Patients with Partial-Thickness Tears: These are tendons that are frayed and damaged but not completely severed. Stem cell therapy can provide the biological signals needed to repair this partial damage and, equally important, prevent progression to a full-thickness tear.
- Individuals with Chronic Tendinopathy: This persistent condition, often called tendonitis, involves tendon degeneration and chronic inflammation. It is especially relevant for those who have not found relief with conservative treatments like physical therapy or cortisone injections. Stem cells can help break the cycle of inflammation and initiate genuine tissue repair.
- Those Seeking to Augment Surgical Repair: For patients who require surgery for a large tear, stem cells can be used as an adjunct. Introducing regenerative cells to the surgical site creates a more robust healing environment, potentially lowering the risk of re-tear and leading to a stronger, more durable outcome.
Understanding When It's Not the Right Fit
Equally important as identifying who can benefit is recognizing when stem cell therapy for a rotator cuff tear is not the optimal first-line treatment. Transparency about these limitations is a critical part of trustworthy medical guidance. Our evaluations are designed to identify these situations early to guide you toward the most appropriate course of action.
A successful outcome begins with an honest assessment. The purpose of a detailed diagnostic evaluation is not just to confirm a diagnosis, but to determine the most effective and direct path to recovery for you.
Here are the key situations where we would typically recommend another approach:
- Complete, Fully Retracted Tears: When a tendon has torn completely and pulled far away from the bone, surgery is almost always required to physically reattach it. Stem cells, while powerful, cannot bridge a large structural gap on their own.
- Active Infections: Any active infection, whether in the shoulder joint or systemic, must be fully resolved before a regenerative procedure can be considered.
- Certain Medical Conditions: Specific health issues, such as hematologic malignancies or certain autoimmune disorders, may make a patient ineligible for autologous stem cell therapy (which uses one's own cells).
Ultimately, determining your candidacy is a collaborative process between you and your physician. It involves a comprehensive review of your MRI or ultrasound, a thorough physical exam, and an open discussion about what this therapy can realistically achieve for your shoulder.
Your Roadmap to Recovery and Long-Term Shoulder Health
Undergoing stem cell therapy for your rotator cuff is a significant first step, but the journey to a healthy, functional shoulder continues beyond the procedure. Lasting success is a partnership between our clinical team and you. Your commitment to a structured post-treatment plan is what transforms the potential of regenerative medicine into tangible, long-term results.
The initial phase is focused on protecting the treated area. This typically involves a brief period of rest to allow the newly introduced stem cells to integrate and begin their work. This is not complete inactivity, but rather mindful movement—avoiding any actions that could disrupt the delicate, early stages of healing.
Building Strength Through Guided Rehabilitation
Following the initial rest period, your recovery transitions to a carefully customized physical therapy program. This is a critical component of your success. The goal is to progressively and safely rebuild strength, restore full range of motion, and improve shoulder stability. Rushing this phase is counterproductive; the objective is to support the regenerating tendon, not overload it.
Our approach to regenerative rehabilitation therapy is designed to work in synergy with your stem cell treatment. Your physical therapist will guide you through exercises that stimulate the healing tendon appropriately, encouraging the new tissue to develop into strong, organized fibers. You can learn more about how we integrate these modalities in our guide on regenerative rehabilitation therapy.
True recovery isn’t just about the absence of pain; it's about restoring confident, functional movement. This guided rehabilitation phase is where that happens, ensuring your shoulder heals stronger and more resilient than before.
Optimizing Your Regenerative Environment
To further enhance your body's healing capacity, we often integrate supportive therapies into your recovery plan. These are selected to create the ideal biological environment for tissue regeneration, ensuring the stem cells have everything they need to function optimally.
One of the most powerful supportive therapies is hyperbaric oxygen therapy (HBOT). By breathing pure oxygen in a pressurized environment, you can dramatically increase the amount of oxygen dissolved in your bloodstream. This oxygen-rich blood then perfuses the healing tissues in your shoulder, providing the essential fuel for cellular repair and new blood vessel formation. This synergy is key to achieving exceptional, lasting shoulder health.
Your Top Questions About Rotator Cuff Stem Cell Therapy
When exploring a new medical treatment, it is natural to have questions. We want you to feel confident and fully informed about the process. Below, we have provided straightforward answers to the most common questions we receive about using stem cells for rotator cuff tears. Our goal is to provide honest, reliable information so you know exactly what to expect.
How Long Until I See Results?
While immediate relief is a common desire, it is important to remember that this therapy is about genuine tissue regeneration—a process that requires time. Some patients report a reduction in pain within the first few weeks, which is largely attributable to the powerful anti-inflammatory effects of the stem cells.
However, the significant structural improvements—those you can feel in your strength and function—typically become noticeable over three to six months. This is the primary window for active tendon healing and remodeling. When paired with a consistent, structured rehabilitation program, these gains can continue to improve for up to a year post-procedure.
Is the Stem Cell Procedure Painful?
Patient comfort is a top priority. Both the harvesting and injection steps are performed with meticulous attention to your comfort, making the experience as seamless as possible.
- Harvesting: Whether we are collecting cells from bone marrow or adipose tissue, the area is thoroughly numbed with a local anesthetic. Patients most commonly report a feeling of pressure, but not pain.
- Injection: We also use a local anesthetic for the injection into the shoulder joint. Because we use precise ultrasound guidance to visualize the target, the procedure is quick and generally very well-tolerated.
It is normal to experience some mild soreness at the injection or harvest site for a few days, but this is typically managed easily without the need for strong pain medication.
Why Choose Mexico for This Therapy?
Choosing a medical destination like San José del Cabo provides access to advanced regenerative protocols that operate within a robust regulatory framework. At Longevity Medical Institute, this allows our physicians to offer comprehensive treatments that may follow different guidelines than those in the U.S. or Canada.
Our treatments are performed exclusively in COFEPRIS-licensed medical facilities, combining the highest standards of care with state-of-the-art cell processing in our on-site, ISO-certified lab.
This integrated approach means you receive physician-led care that is both cost-effective and delivered in a premium, patient-first environment. We manage every aspect of your care, from your initial consultation to long-term follow-up, ensuring your safety, clarity, and continuity of care are prioritized at every step.
Considering Stem Cell Therapy in San José del Cabo?
San José del Cabo is home to Longevity Medical Institute’s primary regenerative medicine clinic, serving patients seeking physician-guided longevity and regenerative therapies in Mexico.
All treatments are delivered within licensed medical facilities and follow defined clinical protocols. Patients considering care in San José del Cabo are supported through consultation, treatment planning, and follow-up to help ensure clarity, safety, and continuity of care. Learn more about our San José del Cabo clinic.
Author
Dr. Kirk Sanford, DC — Founder & CEO, Longevity Medical Institute. Dr. Sanford focuses on patient education in regenerative and longevity medicine, translating complex therapies into clear, practical guidance for patients.
Medical Review
Dr. Félix Porras, MD — Medical Director, Longevity Medical Institute. Dr. Porras provides clinical oversight and medical review to help ensure accuracy, safety context, and alignment with current standards of care.
Last Reviewed: May 24, 2024
Short Disclaimer
This information is for educational purposes only and is not medical advice. It does not replace an evaluation by a qualified healthcare professional. For personalized guidance, please schedule a consultation.