Stem Cell Treatment for Joints: A Patient's Guide to Regenerative Relief
When chronic joint pain becomes a constant companion, it diminishes more than just your physical comfort—it impacts your quality of life, turning simple movements like walking or lifting into daily challenges. Stem cell treatment for joints is an advanced regenerative therapy designed to work in harmony with your body’s innate healing intelligence to address the root cause of the pain.
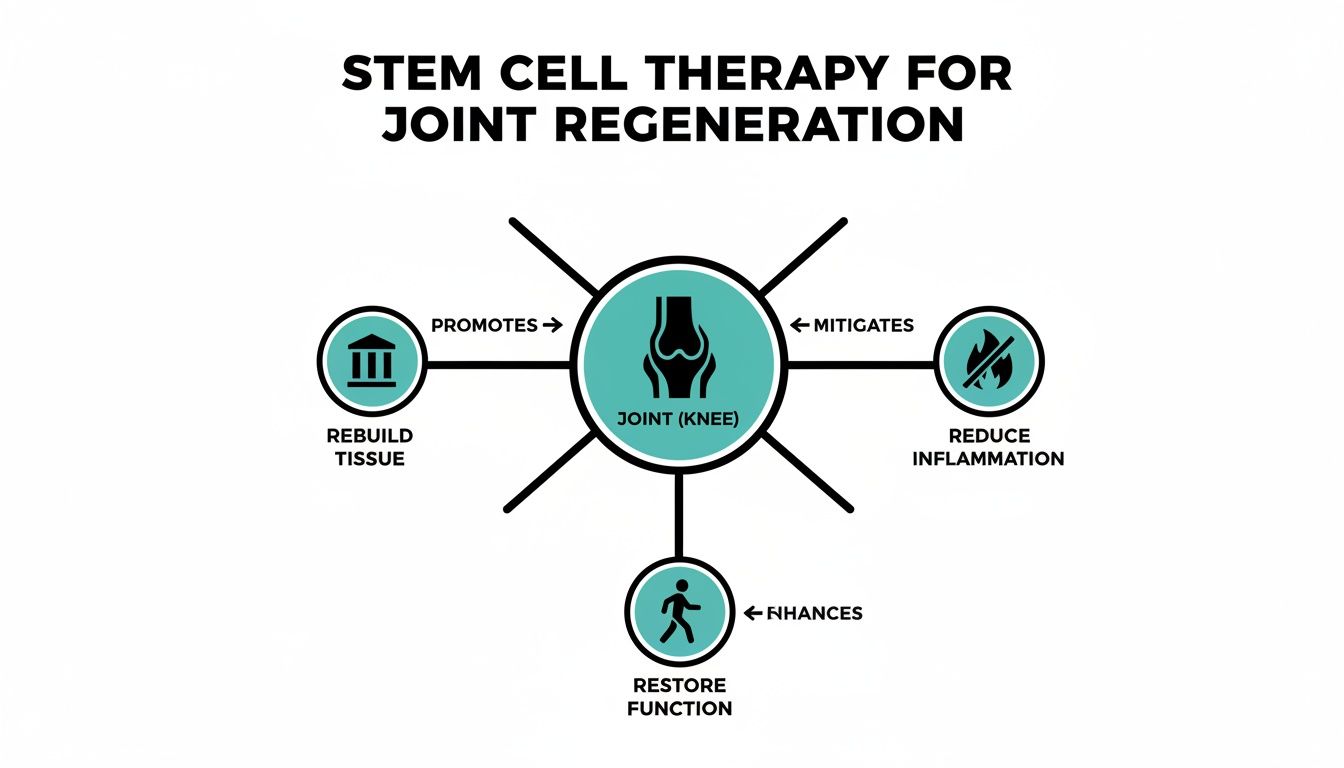
The principle is elegantly simple yet clinically sophisticated: deliver a concentrated population of potent stem cells directly to a damaged joint. The objective is to help calm inflammation, support the rebuilding of worn tissue, and ultimately, restore function and comfort.
How Stem Cell Therapy Works for Joint Pain
For those navigating persistent joint pain from osteoarthritis or a past injury, the cycle of conventional treatments can be frustrating. Traditional approaches often focus on managing symptoms. While pain medications and corticosteroid injections may offer temporary relief, they rarely address the underlying issue. At the other end of the spectrum, total joint replacement is a major surgical intervention requiring significant recovery time.
Stem cell therapy offers a different path forward—one centered on regeneration rather than symptom management.
Think of stem cells as your body’s own elite repair team. These unique cells possess the ability to develop into various tissue types, such as cartilage or bone. More importantly, they function as powerful signaling hubs that orchestrate a complex, localized healing response.
When introduced into a damaged joint, they initiate healing in several key ways:
- Reduce Chronic Inflammation: Stem cells release potent anti-inflammatory signals that help quiet the persistent irritation driving joint pain and degeneration.
- Stimulate Tissue Repair: They secrete growth factors that serve as a catalyst for your own local cells, encouraging them to begin rebuilding damaged cartilage and ligaments.
- Modulate the Immune Response: By helping to balance local immune activity, they foster a healthier, pro-healing environment for long-term joint health.
A Foundational Approach to Healing
This approach is fundamentally different from merely masking pain. It’s about providing your joint with the biological resources it needs to initiate its own repair. Instead of placing a temporary patch on the problem, the goal is to rebuild the joint’s foundation from within.
By addressing the underlying drivers of degeneration, we aim for lasting pain relief and improved mobility. To better understand the science, you can explore our detailed guide on how regenerative medicine works.
Simply put, the objective is true biological improvement. The table below outlines the core goals of this sophisticated approach.
Key Goals of Regenerative Joint Treatment
Therapeutic GoalHow Stem Cells ContributeControl InflammationRelease powerful anti-inflammatory signals to calm the joint environment.Stimulate Tissue GrowthSecrete growth factors that activate local cells to rebuild cartilage and tissue.Reduce PainBy addressing inflammation and degeneration, pain is reduced at its source.Improve FunctionRestored tissue and reduced pain lead to better mobility and joint stability.Slow DegenerationCreating a healthier joint environment helps slow the progression of conditions like osteoarthritis.
The mechanism behind this process relies on mesenchymal stem cells (MSCs), which are central to modern regenerative treatments and have shown notable results in joint repair and arthritis management. The right clinical protocol can help cultivate new joint tissue, potentially delaying or even avoiding the need for major surgery.
By harnessing the body's own regenerative potential, stem cell therapy for joints targets the source of pain and dysfunction. The objective is to facilitate genuine healing and tissue repair, leading to sustained improvements in both comfort and quality of life.
This focus on foundational repair is what distinguishes stem cell treatment as a forward-thinking option for restoring joint health.
The Science of Joint Repair and Regeneration
How do stem cells know precisely where to go and what to do once introduced into a damaged joint? The answer lies in a sophisticated biological communication system. The process is not random; it is a targeted response guided by your body's own intelligent healing mechanisms.
When a joint is injured or affected by a degenerative condition like osteoarthritis, the damaged tissues release chemical distress signals called cytokines. These signals act as a biological beacon, creating a chemical trail that attracts the introduced stem cells directly to the specific site of damage.
Once these powerful mesenchymal stem cells (MSCs) arrive, they do more than act as simple building blocks. They function as master regulators, orchestrating a complex, multi-faceted healing cascade.
The Three Pillars of Cellular Action
The regenerative power of stem cell treatment for joints is centered on three primary functions. The cells work simultaneously to calm the joint environment, signal for repairs, and support tissue rebuilding, creating a truly comprehensive approach to joint restoration.
- Anti-Inflammatory Response: Chronic inflammation is a primary driver of joint pain and tissue breakdown. MSCs release potent anti-inflammatory molecules that interrupt this destructive cycle, calming the joint and creating a more favorable environment for healing.
- Paracrine Signaling: This is where the therapeutic orchestration occurs. Stem cells secrete a host of bioactive molecules, including growth factors and exosomes. These are powerful messengers that "communicate" with your native cells, instructing them to activate, multiply, and begin the work of repairing damaged cartilage, ligaments, and tendons.
- Differentiation Potential: A key characteristic of MSCs is their ability to differentiate, or transform, into specialized cells. When needed, they can develop into chondrocytes—the very cells responsible for creating new cartilage—helping to rebuild the joint's essential cushioning from within.
This infographic helps visualize the core benefits, illustrating how the therapy aims to rebuild tissue, reduce inflammation, and restore overall function.
This multi-pronged approach targets the root causes of joint pain and degeneration rather than just masking symptoms. The goal is to facilitate genuine biological repair that leads to lasting functional improvement.
A Focus on Mesenchymal Stem Cells
The type of cell utilized is critical for achieving optimal outcomes in joint therapy. At Longevity Medical Institute, we utilize MSCs sourced from ethically donated umbilical cord tissue. These are young, vibrant, and highly active cells with robust regenerative capabilities.
The primary role of injected stem cells is not just to replace damaged tissue, but to orchestrate a complex healing process. They act as "conductors" of the cellular symphony, directing the body’s own repair mechanisms to function more effectively and efficiently.
This targeted biological process allows the treatment to be precisely tailored to your specific condition. By enhancing and guiding your body's innate healing abilities, stem cell treatment for joints aims to provide not just temporary relief but a foundational restoration of joint health. For those interested in the specifics of cell sourcing, you can learn more about the benefits of umbilical stem cell therapy.
This intelligent, multi-step process—attraction, modulation, and regeneration—is the science behind how a simple injection can initiate a profound and lasting repair process within your joints.
Which Joint Conditions Can Stem Cells Help?
The true value of any medical therapy lies in its ability to solve real-world problems. For stem cell treatments, this means translating scientific potential into targeted relief for specific, debilitating joint conditions. This is not a one-size-fits-all solution; it is a precise medical intervention, customized to the unique anatomy and degeneration of each joint.
By focusing on the areas that bear the most stress—the knees, shoulders, hips, and spine—we can see how this regenerative strategy addresses the root causes of pain and functional loss. Clinical success depends on precision: delivering the right cells to the exact point of injury.
Treating Knee Pain and Degeneration
The knee is one of the most common sites for joint pain, owing to its constant weight-bearing function and complex structure. For many knee-related issues, stem cell treatment for joints offers a promising alternative to merely managing pain.
- Osteoarthritis: For mild to moderate cases, stem cells can help calm the inflammatory environment and encourage the repair of worn cartilage, leading to reduced pain and improved mobility.
- Meniscus Tears: Small to moderate tears in the meniscus—the knee’s natural shock absorber—can be addressed by promoting healing within the damaged tissue itself.
- Ligament Injuries: For partial tears of ligaments like the ACL or MCL, stem cells can support the body’s own repair mechanisms, potentially strengthening the ligament and improving overall joint stability.
By delivering a concentrated dose of regenerative cells directly into the knee joint, the therapy aims to reset the local environment to a healthier, more functional state. If your primary concern is knee pain, we invite you to explore our detailed guide on stem cell injections for knee pain.
Addressing Shoulder Instability and Pain
The shoulder's remarkable range of motion is also what makes it highly susceptible to injury. Stem cell therapy can be particularly effective for the soft tissue damage common in this complex joint.
We often see excellent results with conditions such as:
- Rotator Cuff Tendinopathy and Tears: For partial tears or chronic inflammation, stem cells can help reduce inflammation and stimulate tendon repair, translating to less pain and improved function.
- Labral Tears: Small tears in the labrum (the cartilage ring that stabilizes the shoulder socket) may benefit from the regenerative signals that stem cells provide.
- Shoulder Osteoarthritis: In cases of mild to moderate arthritis, the therapy can help manage pain and potentially slow the degenerative process.
Restoring Hip Function and Mobility
Hip pain can bring daily life to a halt, making everything from walking to standing a challenge. Stem cell therapy offers a minimally invasive option for addressing the early to moderate stages of several hip conditions.
The goal is to intervene before the joint reaches a "bone-on-bone" state. We aim to provide the body with a biological boost to help its repair systems get ahead of the degenerative curve, preserving the natural joint and potentially avoiding or delaying major surgery.
Key applications for the hip include:
- Hip Osteoarthritis: Targeting inflammation and cartilage wear in the early to moderate stages can bring significant pain relief.
- Labral Tears: Similar to the shoulder, small tears in the hip's labrum can be addressed with regenerative injections.
- Avascular Necrosis (Early Stage): In some early cases, stem cells may help improve blood supply to the bone, supporting its health and structure.
Supporting Spine and Back Health
Chronic back pain is often linked to the breakdown of the discs and joints that support the spine. Stem cell therapy can be used to target the specific source of this degeneration.
- Degenerative Disc Disease: For discs that are losing height and hydration, injections can help reduce local inflammation and potentially improve the disc's cellular health.
- Facet Joint Arthritis: The small facet joints in the spine can develop arthritis just like any other joint. Stem cells can help manage the associated inflammation and pain.
The translation of stem cell science into these clinical applications has advanced rapidly. As of late 2023, there were over 8,400 ongoing clinical trials investigating stem cell applications for hundreds of conditions, with a significant focus on orthopedic issues like osteoarthritis, cartilage repair, and ligament damage. Musculoskeletal medicine is expected to be one of the largest growth areas for these therapies. You can learn more about the extensive clinical trials underway to see the global scope of this research. This ongoing investigation continues to refine how we apply stem cell treatment for joints to achieve the best possible outcomes for our patients.
Your Treatment Journey: From Consultation to Recovery
Deciding to pursue regenerative therapy is a significant step, and you deserve to feel confident and informed throughout the entire process. A successful stem cell treatment for joints is not just about the procedure itself; it is about a meticulously planned experience that supports you from your initial consultation through your full recovery.
This journey is a close partnership between you and our clinical team, where every step is designed for safety, precision, and personalized care.
The Initial Consultation and Candidacy Assessment
The process begins with a thorough clinical evaluation to determine if you are a suitable candidate for this therapy. This is a comprehensive diagnostic deep-dive into your joint health, including a review of your medical history, a discussion of your symptoms, and a detailed physical examination.
Crucially, we utilize advanced diagnostics to see precisely what is happening inside the joint. Tools like MRI and high-resolution ultrasound provide a clear picture of the joint’s condition, revealing the extent of cartilage loss, inflammation, or soft tissue damage. This level of detail allows us to confirm if stem cell therapy is the right tool for your condition and to set realistic, honest expectations for your outcome.
Cell Preparation and Quality Assurance
Once candidacy is confirmed, the next step is preparing the mesenchymal stem cells (MSCs) for your treatment. The success of the therapy hinges on the quality, purity, and viability of these cells—there is no room for compromise.
Our treatments utilize allogeneic MSCs sourced from ethically donated, full-term umbilical cord tissue. These cells are processed in an ISO-certified, COFEPRIS-licensed laboratory that operates under the strictest safety and quality control protocols. Every batch of cells undergoes extensive screening to ensure it is free of contaminants and contains a high concentration of potent, viable stem cells. This commitment to quality is fundamental to patient safety and achieving desired outcomes.
The entire process, from cell sourcing to preparation, is governed by stringent clinical protocols. This ensures that the regenerative product delivered to your joint is of the highest quality, providing the optimal biological resources needed for healing.
The Treatment Procedure: Precision in Action
The procedure itself is a minimally invasive outpatient treatment designed for both precision and patient comfort. On the day of your therapy, we begin by numbing the targeted joint area with a local anesthetic to ensure minimal discomfort.
Using advanced ultrasound guidance, our physician can visualize the internal structures of your joint in real-time. This technology functions like a GPS for the body, allowing for the precise placement of the needle directly into the damaged area—whether it’s a specific lesion in the cartilage, a tear in a tendon, or the inflamed joint capsule itself. This precision is critical for delivering the concentrated dose of stem cells exactly where they can be most effective. The entire injection is typically completed in under an hour.
Recovery and Post-Treatment Care
After the injection, the true healing begins as your body starts utilizing these new cellular resources to repair and rebuild. While the procedure is minimally invasive, a structured recovery plan is essential for achieving the best possible results.
- Initial Rest Period: For the first 48-72 hours, we recommend rest and avoiding strenuous activity. This allows the cells time to settle into the joint environment.
- Gradual Return to Activity: Over the following weeks, we will guide you on a gradual return to your normal routine. Light, low-impact movement is encouraged to promote healthy circulation and joint function.
- Guided Physical Therapy: A personalized physical therapy program is a key component of a successful recovery. We will prescribe specific exercises to help strengthen the muscles supporting the joint, improve stability, and enhance your overall function as the tissue regenerates.
- Follow-Up Consultations: We will schedule follow-up appointments to monitor your progress, assess functional improvements, and make any necessary adjustments to your recovery plan.
Some patients begin to feel initial improvements within a few weeks, but the full regenerative effects build over time. Most people experience significant pain reduction and enhanced mobility between 3 to 6 months as new, healthy tissue forms and chronic inflammation subsides.
Stem Cell Therapy Compared to Traditional Treatments
It is helpful to see how this regenerative approach compares to more conventional options for joint pain. While treatments like steroid injections or joint replacement surgery have their place, stem cell therapy operates on a fundamentally different principle: helping the body heal itself.
The table below highlights the key differences in approach, goals, and recovery.
TreatmentApproachPrimary GoalRecovery TimeStem Cell TherapyBiological; uses cells to signal and direct repair.True tissue regeneration and healing.Weeks to months of gradual improvement.Steroid InjectionsPharmaceutical; uses potent anti-inflammatories.Temporary symptom and pain management.Immediate but short-lived relief.Joint ReplacementSurgical; replaces the damaged joint with a device.Mechanical restoration of joint function.Months of intensive physical rehabilitation.
Ultimately, traditional treatments often focus on managing symptoms or replacing damaged parts. Stem cell therapy aims to change the underlying environment of the joint, shifting it from a state of degeneration to one of regeneration.
Understanding Safety and Clinical Standards
In the field of regenerative medicine, patient safety is paramount. As more individuals explore stem cell treatment for joints, it is crucial to understand what distinguishes a legitimate, physician-led program from a risky or unproven alternative. An informed decision begins with knowing which clinical standards to look for.
The foundation of any safe and effective therapy rests on non-negotiable pillars: the clinic's regulatory standing, the quality of the cells being used, and the medical protocols that guide every step of your care. These factors are even more critical when considering treatment abroad.
The Importance of Licensed Medical Facilities
Your first and most important consideration should be the clinical environment. A legitimate regenerative medicine practice must operate within a licensed medical facility, not an unregulated office. This distinction ensures the clinic is held to high standards for safety, sterility, and direct medical oversight.
In Mexico, for instance, this license is granted by COFEPRIS (the Federal Commission for the Protection against Sanitary Risks), an agency equivalent to the FDA in the United States or Health Canada. A COFEPRIS license is a clear indicator that the facility and its laboratory meet strict national standards for performing medical procedures and handling biological products.
Operating within this regulatory framework is a direct reflection of a clinic’s commitment to patient safety and ethical care. It guarantees that treatments are delivered under medical supervision in an environment designed to protect patient health.
This official oversight is a crucial safeguard, ensuring everything from equipment sterilization to the therapy itself follows defined clinical protocols.
Cell Sourcing and Quality Verification
The next critical component is the quality of the stem cells themselves. The source of the cells and how they are processed and verified directly impacts both their safety and therapeutic potential. At Longevity Medical Institute, we exclusively use mesenchymal stem cells (MSCs) sourced from ethically donated, full-term umbilical cord tissue.
These young, potent cells are processed in a COFEPRIS-licensed, ISO-certified biotechnology laboratory. This dual certification is key:
- ISO Certification: This confirms the lab adheres to international standards for quality management and consistency.
- COFEPRIS Licensing: This ensures the lab complies with Mexico’s stringent regulations for processing biologics.
Every batch of cells undergoes extensive testing for viability, purity, and safety, confirming it is free from contaminants and contains a high concentration of active, therapeutic cells. This multi-layered verification is essential for delivering a reliable and safe stem cell treatment for joints. We have also prepared a comprehensive guide to answer the question, "Is stem cell therapy safe?"
The global stem cell market has seen remarkable growth, reflecting the expanding clinical application of these therapies. In 2025, the market was valued at $19.34 billion and is projected to reach an impressive $79.95 billion by 2034. North America currently holds the largest share, valued at $10.27 billion in 2025, driven by extensive research and development. Discover more insights about the expanding stem cell market on Fortunebusinessinsights.com. This growth makes it more important than ever for patients to choose clinics that uphold the highest scientific and ethical standards.
Frequently Asked Questions
Exploring regenerative medicine is an important decision, and it is natural to have questions. This section provides clear, straightforward answers to the inquiries our patients most frequently have about stem cell therapy, so you can feel confident and well-informed as you consider your options.
We believe a well-informed patient is an empowered patient. Our commitment is to complete transparency, ensuring you feel secure and knowledgeable at every point in your health journey.
How Long Does It Take to See Results From Stem Cell Injections?
The timeline for results is highly individual and depends on your specific condition, the extent of the joint damage, and your body's unique healing response. The regenerative process is not instantaneous; it unfolds as your body’s repair mechanisms are activated.
While some patients report initial improvements within a few weeks, most begin to notice a tangible difference in pain and function between 4 to 8 weeks post-procedure. True tissue regeneration is a gradual process, with the most significant and lasting improvements typically observed from 3 to 6 months as new tissue fully matures and chronic inflammation subsides.
Is Stem Cell Therapy for Joints a Painful Procedure?
We take great care to ensure the procedure is as comfortable as possible. A local anesthetic is used to thoroughly numb the injection site, so most patients report feeling only minor pressure—similar to a standard joint injection.
It is common to experience some mild soreness, stiffness, or minimal swelling in the joint for a few days afterward. This is a positive sign, indicating that your body’s natural healing response has been initiated. This temporary discomfort is typically managed easily with rest and ice.
The goal of a stem cell treatment for joints is not just the injection itself, but initiating a comfortable healing process. Post-procedure discomfort is typically minimal and indicates that the regenerative cascade has begun.
Am I a Good Candidate for Stem Cell Joint Therapy?
Individuals who tend to see the most benefit are those with mild to moderate joint degeneration—such as osteoarthritis—or specific soft tissue injuries to cartilage, ligaments, or tendons. It is often an excellent option for those who have not found lasting relief from more conservative treatments like physical therapy or cortisone injections.
However, candidacy is determined through a comprehensive medical evaluation, not a simple checklist. This process always includes:
- A detailed discussion of your medical history and symptoms.
- A hands-on physical examination of the affected joint.
- Advanced imaging, such as an MRI or ultrasound, to gain a precise understanding of the extent of the damage.
We carefully consider factors like the severity of your condition (severe "bone-on-bone" arthritis may be less responsive), your overall health, and your personal treatment goals to ensure this therapy is the right fit for you.
How Is Stem Cell Therapy Different From PRP Injections?
This is an excellent question, as both are valuable regenerative treatments. The key difference lies in their therapeutic potency and mechanism of action.
Platelet-Rich Plasma (PRP) is derived from your own blood and utilizes a concentration of platelets. These platelets are rich in growth factors that are effective at reducing inflammation and sending initial signals for the body to begin healing. It can be an excellent first-line regenerative option for milder conditions.
Stem cell therapy, in contrast, is a more powerful and comprehensive approach. It uses mesenchymal stem cells (MSCs) which act as the "master coordinators" of healing. They do not just release growth factors; they actively modulate the immune system, provide far more potent anti-inflammatory effects, and have the potential to differentiate into new tissues like cartilage. For more significant joint conditions, we consider stem cell therapy to be the more robust, foundational option for true tissue repair.
Considering Stem Cell Therapy in Los Cabos, Mexico?
Los Cabos, Mexico offers a unique setting for patients seeking advanced regenerative therapies in a medically licensed environment, with convenient access for international travelers.
Longevity Medical Institute’s Los Cabos, Mexico clinics operate under physician oversight and established medical standards, providing regenerative and longevity therapies within a structured clinical framework. Patients benefit from coordinated care, clear eligibility screening, and a focus on safety and outcomes.
Longevity Medical Institute is the only COFEPRIS federally licensed medical clinic and biotechnology laboratory in Los Cabos, Mexico, delivering regulated, science-backed regenerative and longevity care under Mexico’s highest clinical standards.
Learn more about regenerative care in Los Cabos.
Author
Dr. Kirk Sanford, DC — Founder & CEO, Longevity Medical Institute. Dr. Sanford focuses on patient education in regenerative and longevity medicine, translating complex therapies into clear, practical guidance for patients.
Medical Review
Dr. Félix Porras, MD — Medical Director, Longevity Medical Institute. Dr. Porras provides clinical oversight and medical review to help ensure accuracy, safety context, and alignment with current standards of care.
Last Reviewed: January 22, 2026
Short Disclaimer
This information is for educational purposes only and is not medical advice. It does not replace an evaluation by a qualified healthcare professional. For personalized guidance, please schedule a consultation.